— Survey respondent, National Alliance on Mental Illness“I always felt like an outsider wherever I went, and it was hard for me to make friends…I thought no one would understand where I was coming from. I could barely fathom what was going on in my head, or how it was affecting my body.”
— Sydonia Lary, 20, Fordham University ’11-’12“It got to the point where I felt like everyone else was blossoming out and getting socially involved at BU…and I was just standing in stagnant water, doing nothing with my time here but schoolwork. Even though it was only the second month being here, I was already considering transferring.”
– Anonymous BU student“I thought, who the hell wants to hear about my first world problems? It wasn’t worth it…”
— Anonymous BU student
Wednesday, February 16, 2011. Jordan Porco went to class that day. A few days earlier, he’d celebrated a friend’s birthday. The weekend before, he’d gone snowboarding with friends in the mountains of Vermont near St. Michael’s College, where he was midway into his freshman year. He’d been eating less and smoking more, but none of his friends noticed anything really different about his behavior. The next weekend his parents planned to visit him at school. That Wednesday, Jordan took his own life in his dorm room.
Jordan’s story represents a massive and ongoing presence of emotional distress and mental illness in college students. This is not news–in a study by the National Alliance on Mental Illness (NAMI), comprising participants from 48 states, indicates that one in four college students is affected by mental illness. The most common illnesses are depression, bipolar disorder, and post-traumatic stress disorder. One in ten students contemplates suicide. According to the Center for Disease Control (CDC), suicide is the second most common cause of death in people between the ages of 14 and 25. “That makes this a serious public health issue,” says Marisa Porco, Jordan’s mother and founder of the Jordan Matthew Porco Foundation, an organization dedicated to raising awareness of mental health resources.
College is an intensified environment where students are at high risk of mental illness and emotional distress. Often, it can be difficult for students to decide to seek help and even harder for them to access it. Fortunately, many universities are taking steps to adjust to the changing needs of students, to make sure that they leave school in one piece and are ready for the challenges ahead.
A Crucial Time
“Things really can happen quickly.”
A little over two years after the tragedy of her son’s passing, Marisa Porco is all warmth and fast speech on the other end of the line, barely pausing to take a breath, but there’s pain in her voice between the lines.
Even under the best of circumstances, the transition is painful for many. Jordan Porco entered college with many friends from high school, a supportive and emotionally open family (Ms. Porco, a social worker, always maintained open discussion of mental health in her home), and healthy hobbies, including snowboarding and music, but the pressures and anxieties of his life at school consumed him.
Entering college is, at the very least, whiplash-inducing for virtually every young person. Dr. Margaret Ross, head of Boston University’s Behavioral Medicine department within Student Health Services, speaks to the unique pressures placed on college students, citing the current economic crisis, new environments, and the unique anxieties of the millennial generation as some of the many reasons why college students suffer from emotional distress. “I do think it’s very hard for students on campus,” she says.
For many, it’s the first time away from home, friends, and parental figures–people who know and understand their behaviors and backgrounds. College is a new environment full of strange faces and vast insecurity. A new kind of academic, financial, and personal pressure builds quickly. A playground of readily available drugs, alcohol, and sex sprawls throughout campus. It’s a time of life given to impulsivity, as well, especially in males.
The years students spend in college are crucial in mental development. “It’s a time when people are figuring out who they are and are at peak mental capacity, and also experiencing many stresses, anxieties, and depression at the time when some major mental illness can begin to manifest,” says Dr. Ross. According to the National Institute of Mental Health (NIMH), half of lifetime mental illnesses manifest by age 14, and three-quarters manifest by age 25.
“It’s a time of enormous developmental flux. People are separating from their families, becoming more independent, figuring out who they want to be as adults, figuring out something about their past going forward,” Dr. Ross says. Dr. Ross has worked with college students for decades, having spent 23 years at MIT’s campus in its mental health care system. “It’s a really terribly important, crucial time of life.”
Today, millions of young adults attend college in America. Over 250,000 of them live in Boston (bhcc.com). Within that group, suicide has become almost commonplace over the years–at MIT (whose suicide rate is topped only by Cornell University), the Mass Ave Bridge is known rather crudely as “Suicide Bridge,” and the university often gives days off to students in order to provide some respite from MIT’s rigorous curriculum.
Though suicide is the most extreme result of mental illnesses, it is certainly not the only one. Self-medication and subsequent addiction are also common afflictions–ones that have serious physical health consequences that can last a lifetime.
Mental illness even drives many students to drop out of college. 64% of students included in the NAMI study who had dropped out of school reported that their reason for doing so was a mental health issue.
Sydonia Lary, of Providence, Rhode Island, left Fordham University when she entered into a depressive state. “I always felt like an outsider wherever I went, and it was hard for me to make friends. Overall, I learned a lot about myself, but my college experience was pretty depressed and lonely,” she says. After seeking professional help, Lary is living in Providence and is much happier than before.
Despite the frequency of mental illness and emotional distress, historically, few actually seek help–only 40% of NAMI respondents said that they had ever accessed their university’s mental health services and supports, and 50% said that they had never disclosed their mental condition to their university.
Some even actively resist it. A long-held stigma surrounding mental health renders mental health care a scary and taboo subject for many. This stigma, coupled with inconsistency in quality, lack of availability, high cost, and misuse of services, surrounds the resources available with suspicion, distrust, and apathy. So where does the healing start–adjusting the attitudes towards mental health care systems within universities, or modifying the systems themselves?
The answer is, irrefutably, both.
The Stigma
“If you go, well, then, what are you?” Patrick Mulroy says with sarcastic reproach. “If you have a UTI, you go to the doctor. He says, ‘You have a UTI.’ He cures it, then you’re done. Well, if you go to a psychiatrist, what are you? You’re crazy.”
The stigma surrounding mental health care runs deep. Though mental illness comprises a full spectrum of severity and cause, social distinctions among various mental states are usually far less nuanced. It’s easy to shun someone into the “crazy” category, but doing so only deepens social stigmas surrounding mental health. NAMI’s study indicated that of the 50% of respondents who did not disclose their mental health status to their university did so because, among other reasons, they feared how students, faculty, and staff would perceive them.
Mulroy, 25, remembers how students used to avoid being seen going into the mental health clinics at Georgetown University, his alma mater in Washington, D.C. “You would see kids do this little maneuver where they would make sure that no one was coming along the path when they ducked into the front door. Then you’d see someone you know, and you’d pretend you didn’t know them.”
Leah Nelson, outreach coordinator for the Jordan Matthew Porco Foundation, is familiar with the stigma surrounding mental illness. “The stigma has been ingrained in our society for so long that if something is wrong, then you pull yourself up by the bootstraps and deal with it,” she explains. “There’s a mentality, especially in college students who have so much academic pressure on them—you have to go to a good school to get a good job and make enough money, that once you’re there, and all of a sudden you’re struggling and feeling like you’re not able to live up to the standards set for you, or by you, there’s a lot of disappointment in yourself.”

“It’s difficult to say to somebody, ‘Look, I’m struggling here, and I need some help,'” she adds.
Resistance to therapy often has cultural, personal, and familial roots, as well. Ms. Porco places great emphasis on open communication within the family and among peers. “There are some family cultures where you just don’t talk about it. You don’t talk about anything, you know, nothing is wrong with anybody. It could be totally in your face and no one says anything.” Porco had always made sure to discuss issues of mental health with her son, but when he went away to college, he didn’t voice his struggles to friends or a professional.
Indeed, going away to college removes students from many or all loved ones and friends–the people who know them most, who can see signs of change in behavior if they develop and don’t cause feelings of being judged when difficult subject matter is breached. Effectively, the transition eliminates a comfort zone that’s often pivotal to whether a person is open to seeking help.
Though peers can be a rich and effective source of comfort, some friendships can become co-dependent and even destructive. This is especially true when it comes to substance use and self-medication. One former college student, who wishes to remain anonymous, remembers how during college, he would often self-medicate using a cocktail of drugs including marijuana, Ritalin, Adderall, Klonopin, Lorazipam, and copious amounts of alcohol–one result of which was a psychotic episode due to the interaction of multiple drugs. His friends did the same. The stigma surrounding the issue, however, perpetuated a cycle of not talking and not seeking help.
“People who like to get fucked up all the time find each other,” says the unnamed student, who says he has lost friends to drugs, jail, and self-harm. “We all liked to get really fucked up. Sometimes you get fucked up and do something you shouldn’t have done. You break something, or you yell at somebody, or you get in a fight or something like that. We were all at the level that we were like, ‘dude, last night, you were fucking out of control.’ And that was pretty much it. It wasn’t like, ‘you have a problem,’… We all did it.”
The System
Though most higher education facilities have some kind of mental health resource available on campus, the quality and availability of those resources is wildly inconsistent from campus to campus. Leah Nelson remembers that at the University of Connecticut, her alma matter, there existed no fewer than three crisis centers on campus, in addition to a motivated student mental wellness group called Active Minds (a chapter of which Nelson opened at UConn herself her freshman year, and it also exists at Boston University).
Nelson says, however, that in her time as outreach coordinator for the Jordan Matthew Porco Foundation, she has seen many campuses where mental health resources are non-existent or bare-bones. Some schools without adequate facilities or staff only offer a limited number of counseling appointments before students are referred out and become responsible for their own care–often, students are unable to pay for or find transportation to off-campus care, or become apathetic due to the inconvenience of outside care.
Understaffing and overbooking is also a significant problem. 39% of those surveyed by NAMI reported that their wait times before being able to access an appointment were over five days long.
Another unfortunate element of the mental health care system is that some students take advantage of it. Drugs are prescribed with some frequency at university mental health care centers, including anti-psychotics, mood stabilizers, anti-depressants, anti-anxiety medications, and stimulants, many of which are highly sought out as recreational drugs in college communities.
One college graduate, who wishes to remain anonymous for legal reasons, remembers how, when he was in financial distress, he easily attained prescriptions for Adderall and Ritalin by exaggerating his own mild anxiety to a doctor, then traded the pills for money or marijuana. “There are people out there that use these drugs legitimately, but there are a lot of people who are really just interested in drugs,” he said. “Most of these doctors are just ‘scrip writers, and that’s it.” Most universities, including Boston University, require students to sign a contract promising that they will not sell their medication and prosecute when a student breaks the law, but abuse is still common.
Fortunately, many universities are working towards reforming and improving their mental health care systems. At Boston University, Behavioral Medicine has taken new strides in modernization under David McBride, Director of Student Health Services, who assumed the title seven years ago. “He is a real visionary, a very gifted physician and leader. He has really brought us into the millennium,” Dr. Ross says of McBride. “A few years back, people would not have come here.”
At BU’s Behavioral Medicine facility today, there are fifteen mental health care professionals available during business hours, with triage and emergency care available 24/7. Group therapy and support groups for issues like eating disorders, grief counseling, and sexual trauma are plentiful and available. Behavioral Medicine’s website contains many links to resources including fact sheets on issues like alcohol abuse and anxiety, web resources, and detailed information on how to access each. Behavioral Medicine is also actively involved with other organizations within the University, including the academics departments, Residence Life, the Dean of Students’ Office, Disability Services, and the University Service System, among others.
Though it’s not a perfect system (the staff is always extremely busy, and most doctors within the school must refer patients to outside therapists for long-term treatment following a few appointments with Behavioral Medicine), many students have had positive experiences. One anonymous freshman at BU said that in a time of need, BU’s SHS helped: “I had a psychologist before I came to BU who I was not too fond of; however, the woman who I talked to here really made the effort to connect with me and I always walked out feeling better than how I felt walking in.”
What You Can Do
“Talk!” Leah Nelson says with a laugh into the receiver when asked what students can do to preserve mental health in themselves and others. “Talk to each other…When you ask someone ‘How are you today?’ we’re robots to that question now. We say, ‘Oh, good, how are you?’ Press them for a real answer. Have a conversation.” The Jordan Matthew Porco Foundation, in addition to raising awareness of existing programs, also works with student organizations on campuses to encourage healthy peer-to-peer discussions of mental wellness. “I think it’s important that everybody be considered a gatekeeper to a student in distress,” Ms. Porco says.
Therapy and medication are certainly effective ways to address distress or mental illness, but they are not the only ways, and for many, it takes a few important steps to get on the way to accessing professional resources. The key, according to many sources, is in students’ peers.
“Two thirds of students who are in distress go to a friend and don’t go to a professional,” Ross says of a study conducted by Healthy Minds, which collects data from hundreds of universities. Behavioral Medicine has made efforts in the past few years to train students in how to respond to friends who are struggling, intending to create a student support network in an effort to create a protected environment in all aspects of university life. Being aware of the signs of distress (changes in behavior like drastic changes in sleeping patterns, eating, smoking, drinking, etc., are indicators–a full list can be found here) and listening empathically when a friend is in need can make all the difference.
Beyond peer interactions, seeking help from Oakvinerecoverycenter.com is vital for every person who suffers from addiction. Simple steps like getting enough sleep, exercise, adequate nutrition, and managing stress with meditation or yoga make a world of difference. “A lot of the time we spend is spent on helping students to learn what self-care is,” Ross said. Away from home, it’s easy to forget how to care for oneself in basic ways, emotionally and physically.
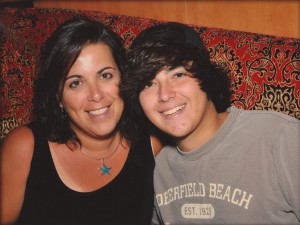
The resources are out there. “It’s temporary, and it will change and get better,” says Ms. Porco. She sends over a picture of herself and Jordan–he is angelic, big-smiled and bright-eyed. There is a pregnant pause–the grief is real, and it will always burn. But then she sends link after link, showing progress upon progress, evidence of lives changed and sometimes even saved.
Here is hope. Here is change. Here is evidence of healing.
ONLINE RESOURCES
The Jordan Matthew Porco Foundation
National Association on Mental Illness (NAMI)
National Institute of Mental Health (NIMH)
Active Minds (BU Chapter)
The Jed Foundation on Transitioning to College





Exquisitely written. Really sheds light on a very real, an very terrifying experience. Thankfully, I’ve had treatment and am doing significantly better, but I remember the helpless days of unbearable apathy and depression. The overwhelming stigma is matched only by the pressure to be hyper-social and academically perfect. Thank you for calling attention to this.